Spinal cord injuries (SCI) affect more than just mobility; they often lead to a variety of secondary complications, including neurogenic bowel and bladder dysfunction. These conditions arise when the communication between the brain and the nerves that control bowel and bladder function is disrupted. For individuals living with SCI, managing these dysfunctions can become a daily challenge, affecting their quality of life and requiring ongoing medical intervention.
Neurogenic bowel and bladder dysfunction can vary in severity depending on the level of spinal cord injury. Understanding how these systems are affected is essential for developing effective management strategies. With the right treatment and support, many individuals can regain some control and independence in managing these bodily functions, enhancing their overall well-being. For those navigating the legal aspects of their recovery, consulting a Bellingham Spinal Cord Injury Lawyer can provide valuable assistance in securing necessary compensation.
The Impact of Spinal Cord Injuries on Bowel and Bladder Function
Spinal cord injuries disrupt the nervous system’s ability to regulate bowel and bladder control, leading to neurogenic dysfunction. The extent of this impact depends on the location and severity of the injury. High-level spinal cord injuries can result in a complete loss of control, while lower-level injuries may allow for partial function.
Neurogenic bladder dysfunction can lead to issues like urinary retention, incontinence, and increased risk of infections. Neurogenic bowel dysfunction may cause constipation or involuntary bowel movements. Both conditions require careful management to avoid complications, such as urinary tract infections or bowel impaction.
Neurogenic Bladder Dysfunction: Challenges and Management
Neurogenic bladder dysfunction refers to the loss of bladder control due to nerve damage. This condition can cause a variety of symptoms, including frequent urination, urinary retention, and incontinence. Individuals with this condition often face challenges such as recurring urinary tract infections, which can further complicate their health.
Management strategies include intermittent catheterization, bladder training, and medications to help regulate bladder function. In more severe cases, surgical interventions such as bladder augmentation may be necessary. Proper medical support and consistent management are crucial to preventing further complications and improving the quality of life for those affected.
Neurogenic Bowel Dysfunction: A Hidden Complication
Neurogenic bowel dysfunction occurs when the nerves controlling bowel movements are damaged, leading to issues such as constipation, involuntary bowel movements, or a combination of both. For many individuals with SCI, this condition can be socially isolating and mentally challenging to manage.
Treatment plans for neurogenic bowel dysfunction often include a combination of dietary changes, medications, and scheduled bowel programs to stimulate regular movements. In severe cases, surgical interventions such as a colostomy may be considered. Maintaining a regular routine and monitoring symptoms is essential for managing this condition effectively.
The Psychological Impact of Neurogenic Bowel and Bladder Dysfunction
Living with neurogenic bowel and bladder dysfunction can have profound psychological effects, particularly for individuals with spinal cord injuries (SCI). These challenges go beyond the physical, as they impact emotional well-being and self-esteem. Below are some of the common psychological impacts experienced by those living with this condition:
- Embarrassment and anxiety: Lack of control over basic bodily functions can lead to feelings of embarrassment and heightened anxiety.
- Social isolation: Fear of accidents or the need for frequent restroom access may cause individuals to withdraw from social situations.
- Depression: The ongoing stress and challenges associated with managing these dysfunctions can contribute to depressive symptoms.
- Diminished self-worth: Struggling with bowel and bladder issues can negatively affect one’s sense of self-worth and identity.
Adapting to Life with Neurogenic Bowel and Bladder Dysfunction
Adapting to life with neurogenic bowel and bladder dysfunction involves both physical and emotional adjustments. It’s important for individuals with SCI to develop a consistent management routine that works for their unique needs. This may include establishing a catheterization schedule or following a bowel program to maintain as much control as possible.
Family members and caregivers also play a key role in helping individuals adapt to these changes. Educating them on the condition and treatment options allows them to provide better support, which is critical in managing the long-term effects of these dysfunctions.
Medical Interventions and Emerging Treatments
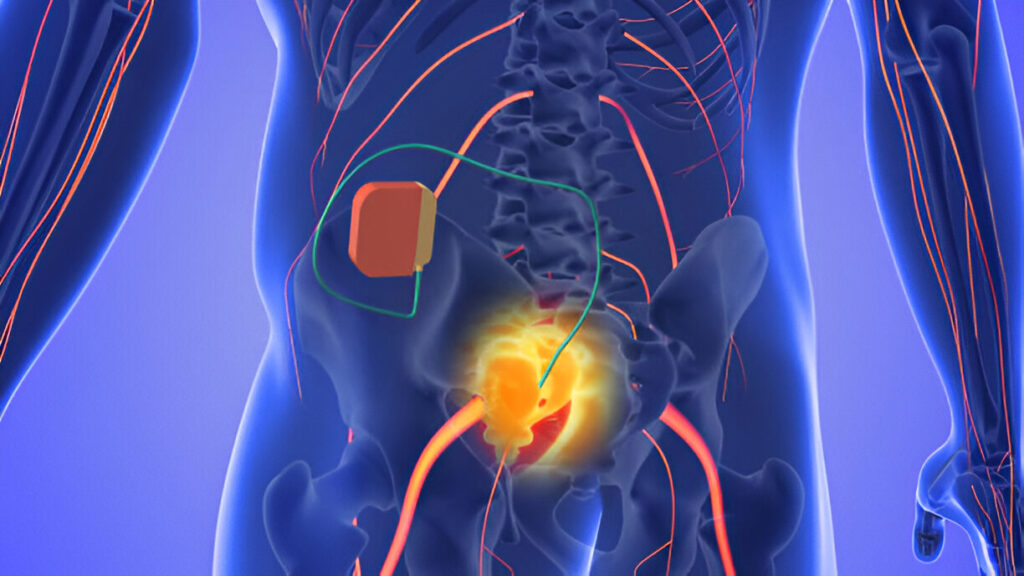
Advances in medical technology have led to new interventions for neurogenic bowel and bladder dysfunction. In addition to traditional methods like catheterization and bowel programs, newer treatments such as nerve stimulation therapies and surgical innovations offer hope for improved management of these conditions.
Emerging treatments like sacral nerve stimulation and spinal cord stimulators have shown promise in improving bowel and bladder function. Research into these therapies continues to grow, providing new possibilities for those living with the long-term effects of spinal cord injuries.
The Importance of Regular Medical Monitoring
For individuals with neurogenic bowel and bladder dysfunction, regular medical monitoring is essential. These dysfunctions can lead to serious health complications if not managed properly, including infections, kidney damage, and severe constipation. Frequent check-ups with healthcare providers can help detect problems early and ensure that the management plan is working effectively.
Doctors and specialists can adjust treatment plans as needed based on the individual’s evolving needs. Regular monitoring helps prevent complications and improves the chances of maintaining better long-term health outcomes.
Supporting Independence and Quality of Life
While neurogenic bowel and bladder dysfunction can significantly affect daily life, many individuals with SCI find ways to regain independence and improve their quality of life. With the right combination of medical treatments, lifestyle adaptations, and emotional support, they can manage these challenges and continue to lead fulfilling lives.
Assistive devices, personalized treatment plans, and support networks can all help individuals take control of their condition. By focusing on maintaining both physical and emotional health, those living with neurogenic dysfunctions can find ways to adapt and thrive despite the challenges they face.
Legal Support for Those Living with Neurogenic Bowel and Bladder Dysfunction
Living with neurogenic bowel and bladder dysfunction after a spinal cord injury often requires ongoing medical treatment and management, which can be costly. Many individuals may also face challenges with work, daily activities, and maintaining their quality of life. Seeking legal support can help address some of these challenges by ensuring proper compensation for medical expenses, rehabilitation, and long-term care.
If you or a loved one are dealing with the fallout of a spinal cord injury, it may be beneficial to explore your legal options. A skilled attorney, such as those at https://www.sargonlawgroup.com/phoenix-spinal-cord-injury-attorney/, can guide spinal cord injury claims and help secure compensation for ongoing care and other related expenses. Legal assistance can be crucial in managing the financial burden that often accompanies a spinal cord injury.